Case• 44. Management of anticoagulation
SUMMARY
A 60-year-old man presents to you in your general dental practice requiring a dental extraction. He is taking oral anticoagulants. How will you deal with his extraction?
History
Complaint
The patient has a broken-down upper first molar that is tender on biting. The patient points directly at the tooth and requests extraction.
History of complaint
The tooth has been root-filled and crowned, but is tender to percussion. There have been several episodes of similar pain in the past year. The crown has been lost from the tooth.
Medical history
The patient reports that he had rheumatic fever as a child and as a result of cardiac valve damage he received a prosthetic heart valve 7 years ago. He is taking warfarin (9 mg daily) and co-amilofruse (amiloride/furosemide diuretic combination; 2 tablets daily). The patient carries an anticoagulation card from his local clinic showing that his international normalized ratio (INR) prothrombin time is usually between 3.5 and 4.5 (Figure 44.1). It was last checked 10 days ago, when it was 3.9.
▪ How does warfarin work and how is anticoagulation monitored?
Warfarin is a vitamin K antagonist. It prevents the liver from utilizing vitamin K to make clotting factors II, VII, IX and X. The patient is usually under the care of an anticoagulation clinic, although some patients are monitored by their GP. Blood tests are performed regularly and the results and drug doses are recorded in a yellow book that the patient should always carry.
▪ What is the INR test, what is its normal therapeutic range and how should the result be interpreted?
The INR is a standardized method of presenting the result of a prothrombin time test. The result is the ratio of the patient’s prothrombin time to that of a standardized control and measures the effectiveness of the extrinsic and common pathways of blood coagulation, those most affected by warfarin. The therapeutic range for patients who have had deep-vein thrombosis or pulmonary embolism is 2.5–3.5. For patients with a prosthetic heart valve it is 3.5–4.5, depending on valve type, at the top of the therapeutic range.
In theory the INR is a standardized test using an internationally accepted standard. Unfortunately, in practice accurate standardization of the INR is often not reproducible, and small changes in the decimal places of the result cannot be relied upon to reflect small changes in anticoagulation. The test should be regarded as an estimate of anticoagulation rather than an accurate measure.
▪ Is this patient at risk of infective endocarditis?
Yes, all patients with the following conditions are considered at risk and a prosthetic heart valve is a relatively high risk factor that carries a very high risk of fatal outcome if endocarditis develops:
• Acquired valvular heart disease with stenosis or regurgitation
• Surgically corrected or altered congenital heart defects*
• Previous infective endocarditis
• Hypertrophic cardiomyopathy.
 |
| Fig. 44.1 |
Examination
Extraoral examination
No lymphadenopathy is present and the extraoral examination reveals no abnormalities. However, a large bruise is apparent on the patient’s right forearm, consistent with the degree of anticoagulation.
Intraoral examination
The patient has a number of teeth with large restorations and several crowned teeth. His periodontal condition and oral hygiene are relatively good with only small amounts of detectable interdental plaque.
The upper first molar tooth is broken down. Root-filling material can be seen in the open pulp chamber and much of the root surface is carious. The tooth is tender to percussion. The second premolar is not tender to percussion but produces a dull percussive note. No sinus is present. The periodontal condition seems reasonable and there is no significant bone loss around the tooth on probing.
There is caries around the distal margin of a crown on the first premolar.
Investigations
▪ What investigations are required and why?
The premolars and molars should be checked for vitality. The first premolar is vital but both second premolar and first molar do not respond to testing with an electric pulp tester. A radiograph is required in order to decide whether the molar is restorable, that is, to gauge the extent of caries and determine the success of the root filling. If extraction turns out to be required, a radiograph will be necessary to assess the difficulty of the extraction. This is particularly important in a patient who may suffer prolonged bleeding. A periapical view is the ideal view.
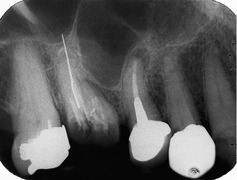
▪ The periapical view is shown inFigure 44.2. What does it show?
The first permanent molar is extensively carious. A root filling is present but only one gutta percha or silver point is visible, in the palatal canal. It extends beyond the apex by approximately 2 mm. The buccal roots are not clearly visible but appear to contain no root filling. The overextended root filling lies close to the antrum and the antrum extends down between the roots of the first molar and second premolar. There is no apical radiolucency. The second premolar is also root-filled. The root filling appears to stop just short of the anatomical apex at an appropriate point but a small apical radiolucency is present, surrounded by the lamina dura of the tooth socket. The caries below the crown on the first premolar is visible and the second molar contains a large pinned amalgam.
Diagnosis
▪ What is your diagnosis? Explain your diagnosis.
The patient’s pain is caused by periapical periodontitis of the first permanent molar.
The patient points clearly to this tooth as the cause of his pain. This and the tenderness on percussion indicate inflammation of the periodontal ligament and the overfilled root canal provides a likely cause. No radiolucency is shown on the radiograph. However, none is required for diagnosis in the presence of typical signs and symptoms. There may be either only a small apical lesion or one on the apices of the buccal roots or in the trifurcation, both of which are superimposed on the film.
The second premolar has an unsuccessful root filling and small periapical radiolucency, almost certainly a periapical granuloma. However, it is not tender to percussion and is not felt to be the cause of the pain by the patient. The first premolar is vital and the caries would produce pain of pulpitis type without tenderness on biting or percussion.
Treatment
▪ What treatment would you recommend?
The primary consideration should be that the patient is at risk of infective endocarditis and potential sources of infection should be eradicated. The first molar cannot be restored without another root filling and extensive preparation. The patient prefers extraction and this is the appropriate course of action. The first premolar is more problematic. It appears to be symptom-free and the apical granuloma has probably been present for some time. This lesion is a further potential source of infection and it must be eliminated, either by extraction or another root filling. The success of the new root filling must be monitored to ensure that it is successful and if not, either apicectomy or extraction will need to be considered. Treatment may be complicated by the anticoagulation, so there must be a comprehensive treatment plan that takes the rest of the/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses